Slide Show - Managing and Treating MDS-related Anemia
This slide show explains the current management and treatment approaches for MDS-related anemia. It provides an overview of blood transfusions, medicines to increase red blood cell production, chemotherapy, future treatments, and bone marrow (stem cell) transplant. Treatment for MDS-related anemia depends on several factors including what type of MDS you have, your general health, your age, your risk score, and what you want for the future.
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about MDS which will help other patients, caregivers and families.
Animation - Managing and Treating MDS-related Anemia
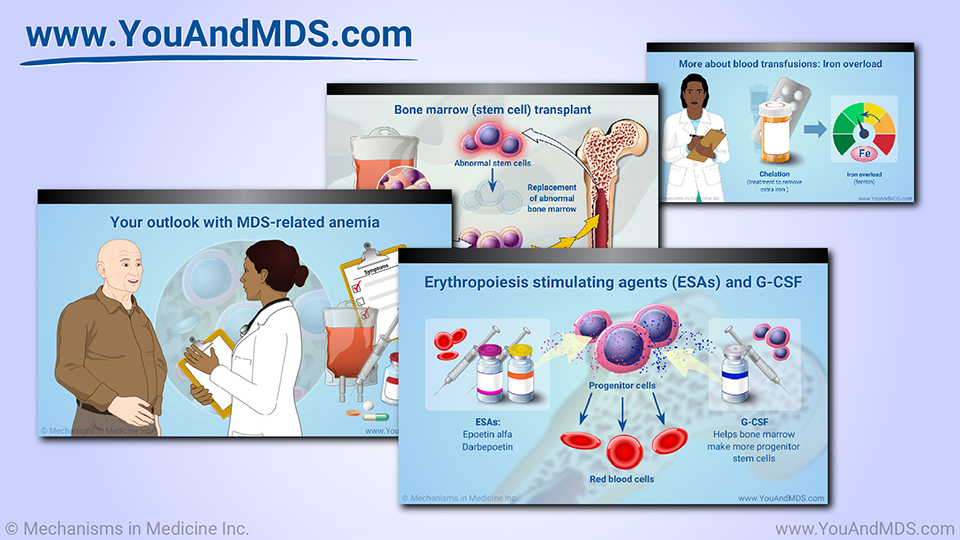
Slide Show - Managing and Treating MDS-related Anemia

1.
What are the treatment options for MDS-related anemia?

2.
What are the goals of treatment for MDS-related anemia?

3.
How is higher-risk MDS-related anemia treated?

4.
What is “refractory anemia” and “primary anemia”? Are these terms still in use?

5.
When do people with MDS-related anemia need blood transfusions?

6.
How often could I need a blood transfusion for MDS-related anemia?

7.
Are blood transfusions safe? Are there risks?

8.
What is iron overload, and how it is treated?

9.
Can my bone marrow return to normal and produce its own red blood cells?

10.
What new treatments are in development for MDS-related anemia?

11.
Are there clinical trials for MDS-related anemia? What does the future hold?

12.
What treatment questions should I ask my doctor about my MDS?

13.
When is a blood and marrow transplant (stem cell transplant) used for MDS-related anemia?
14.
Abby’s story: What has been the biggest challenge with your MDS-related anemia?

15.
Barry’s story: What has been the biggest challenge with your MDS-related anemia?

16.
Bill’s story: What has been the biggest challenge with your MDS-related anemia?
17.
Abby’s story: What has been the greatest success and greatest challenge with your MDS-related Anemia treatment?
18.
Barry’s story: What has been the greatest success and greatest challenge with your MDS-related Anemia treatment?
19.
Bill’s story: What has been the greatest success and greatest challenge with your MDS-related Anemia treatment?
20.
Abby’s story: What advice do you have for other patients on their journey with MDS-related anemia?
21.
Barry’s story: What advice do you have for other patients on their journey with MDS-related anemia?
22.
Bill’s story: What advice do you have for other patients on their journey with MDS-related anemia?